Behavioral Health Integration is a CMS initiative that promotes collaboration between primary care and behavioral health services. Designed for patients with behavioral health conditions (like depression, anxiety, or substance use disorders), BHI helps integrate mental health support into routine care, all while generating additional reimbursement for your practice.
Behavioral Health Integration
Behavioral Health Integration (BHI) Primer
Bridge the gap between mental and physical health with a fully managed BHI program.
- Improve Outcomes
- Enhance Care
- Boost Revenue
What Is Behavioral Health Integration (BHI) ?
Our Fully Managed BHI Workflow:
1. EHR Screening & Patient Identification
We identify patients with qualifying conditions and recent qualifying visits.
Focus on those with ongoing behavioral health needs who benefit from coordinated care.
2. Patient Education & Enrollment
Our team explains the BHI program to patients and secures verbal consent.
Enrollment is handled under your practice name and protocols.
3. Initial Behavioral Health Assessment
A detailed intake consultation to understand the patient’s behavioral and emotional health status.
Establish goals, symptom tracking plans, and care preferences.
4. Monthly Collaborative Care
The Behavioral Health Care Manager coordinates with your primary care team.
Includes monthly follow-ups, care plan adjustments, and coaching.
5. Documentation & Reimbursement Support
All services are tracked in real-time.
Our software generates detailed billing summaries, complete with appropriate CPT codes.
How It Works (In Plain English)
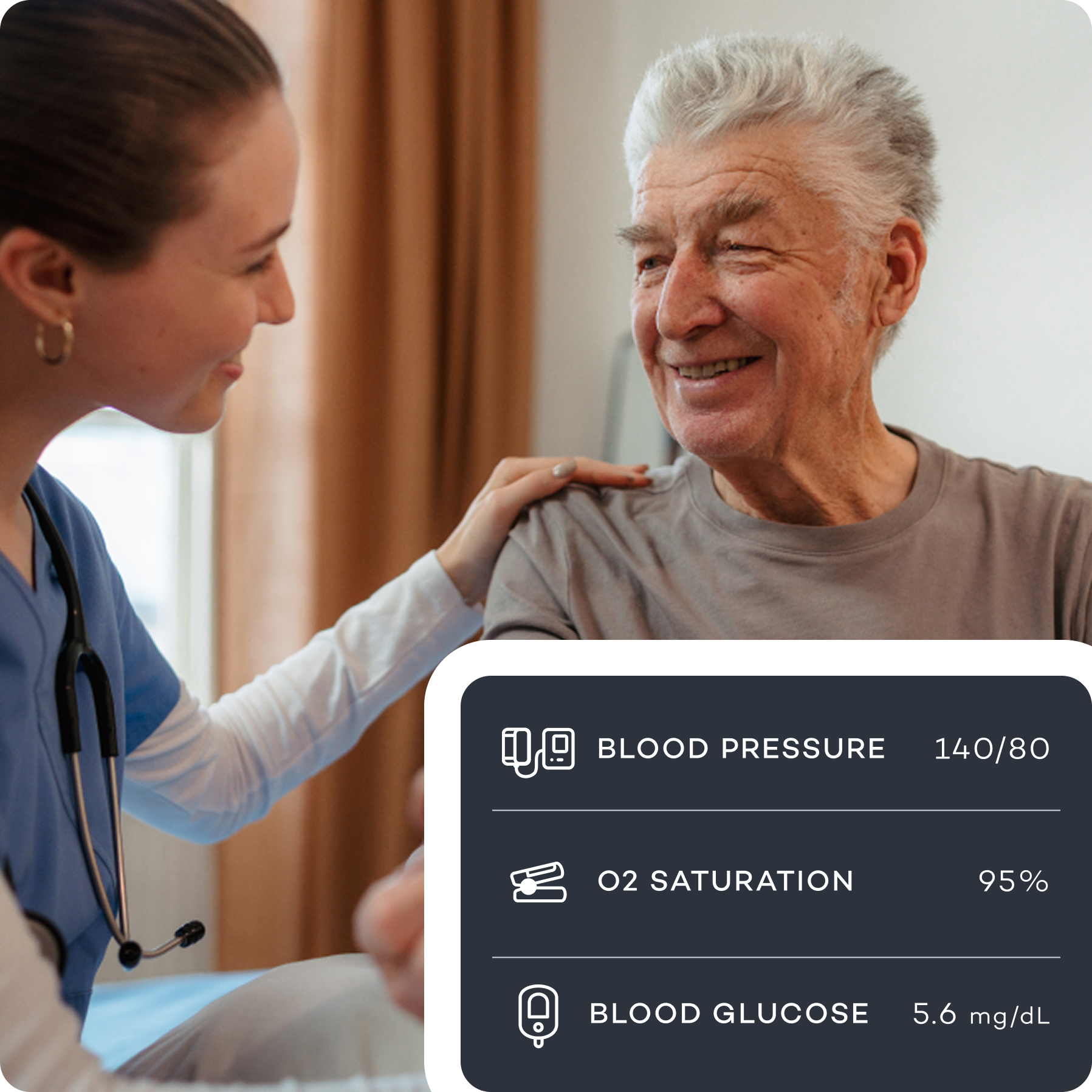
Your patients use easy-to-use medical devices at home—like a blood pressure cuff or glucose meter.
No apps, no setup—the device automatically sends the readings to our platform.
Your staff can see the data in real-time, check on any issues, and spend a few minutes each month reviewing it with the patient.
Our platform tracks everything, makes sure you’re compliant, and at the end of the month—you bill Medicare and get paid. Simple for the patient. Easy for your team. Revenue for your practice.
Frequently Asked Questions
How long does onboarding take?
Once we receive your patient list or EHR access, we can begin outreach within 7 days. Most clinics are fully live within one week.
Why is there an initiation fee?
The fee covers the setup of a HIPAA-compliant database, eligibility screening, and patient enrollment — all critical work done before we generate billable service time.
Why do you need EHR access?
EHR access lets us document directly, improving compliance, audit readiness, and continuity. If preferred, we can also work from a patient panel in Excel format.
How do we bill for services?
We send monthly time logs, care summaries, and superbills. You can submit these to your billing team or we can coordinate directly with them for smoother reimbursement.
What if patients don’t answer?
We make multiple call attempts per month, including after-hours and weekends if needed. Every outreach is logged and counted toward CMS billing thresholds.
Should we start with RPM or CCM?
We recommend starting with CCM due to simpler setup. RPM and other coordination services can be added once workflows are established.
How do you ensure compliance?
All calls are recorded. Our licensed team follows CMS and HIPAA standards for every service, with monthly reporting and documentation for audit-readiness.
What happens if we stop working together?
You’ll retain full access to all care summaries and patient data. That said, we’re confident you and your patients will love the program—so we don’t expect you’ll need to stop.
Increase your RPM revenue today
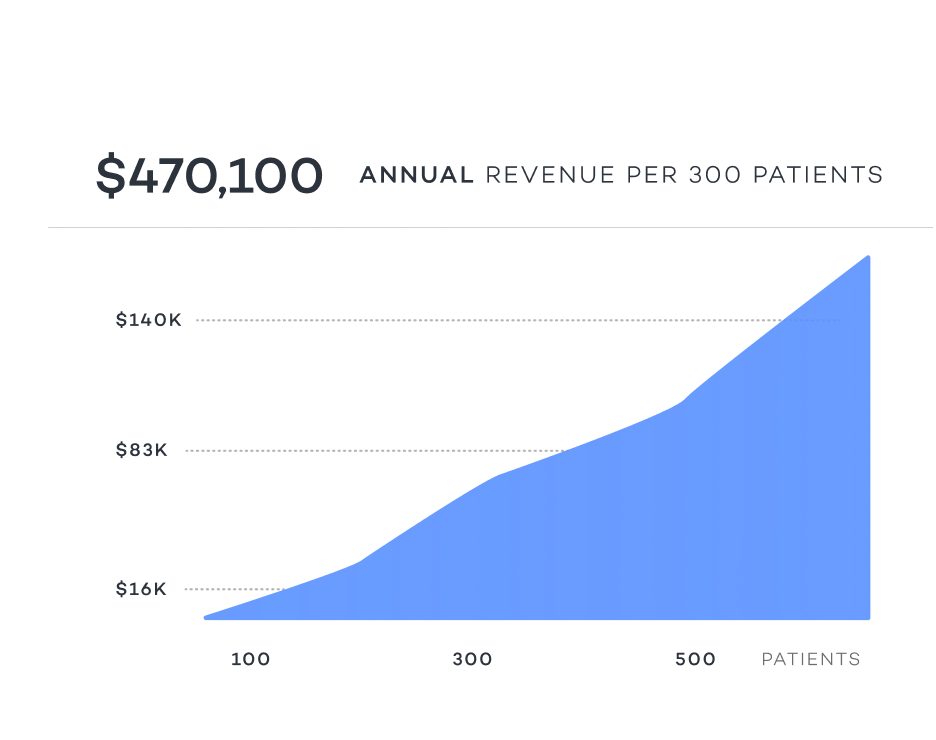
CPT 99453(~$19) Initial Device Setup
This is a one-time billable service for setting up a remote monitoring device (like a blood pressure cuff) and teaching the patient how to use it. It’s billed once at the beginning of care.
CPT 99454(~$43) Device Data Transmission
This monthly billable code covers the supply of the device and the automatic transmission of health data (e.g., at least 16 days of readings in a 30-day period). It’s billed every 30 days as long as the device is active and transmitting.
CPT 99457(~$48) 20-Minute RPM Monitoring & Communication
This is billed monthly when clinical staff or the provider spends 20 minutes reviewing the patient’s data and interacting with the patient in real time. It must include live communication (e.g., phone or video call).
CPT 99458(~$38) Each Additional 20 Minutes
This add-on code is billed alongside 99457 when more than 20 minutes of monitoring and communication is provided in the same calendar month
Why Choose RLH Health?
Instant EHR Integration
Automatically sync patient data directly into your existing workflow—no manual entry required.
Transparent Billing Guidance
Know exactly what CPT codes apply, why they apply, and how to maximize your reimbursements.
Rapid Onboarding
Go from discovery to billing within a single week. No delays, no hassles.
Zero Risk & No Cost
All devices, training, and integration are completely free. You pay nothing upfront.
Clinic Onboarding Checklist
Understanding the process
01
Agreements Submitted
- Send back your signed Services Agreement and BAA to begin onboarding.
- We’ll begin initial processes and lock your clinic into our Week 1 launch window.
02
Panel or EHR Access
- Upload a list of active patients or grant EHR access.
- We’ll use this to identify and enroll eligible individuals.
03
Dedicated Care Line Setup
- We’ll activate and configure your clinic’s outbound patient line.
- This number will be used by our care team for monthly outreach.
04
Clinic Contact Assigned
- Let us know who we’ll coordinate with during onboarding.
- This person will receive updates, reports, and care alerts.
05
Patient Outreach Begins
- Our team begins calling eligible patients within 7 days of onboarding.
- All calls are recorded and made from your branded clinic line.
06
Billing & Care Summaries
- We’ll upload monthly time logs, care summaries, and a detailed superbill.
- We can work directly with your billing team to ensure proper reimbursement
Ready to Start?
Schedule your quick, no-obligation discovery call today—and start billing CCM, RPM, PCM, or BHI within your first 30 days.